Lymphedema treatment: the angiologist’s role
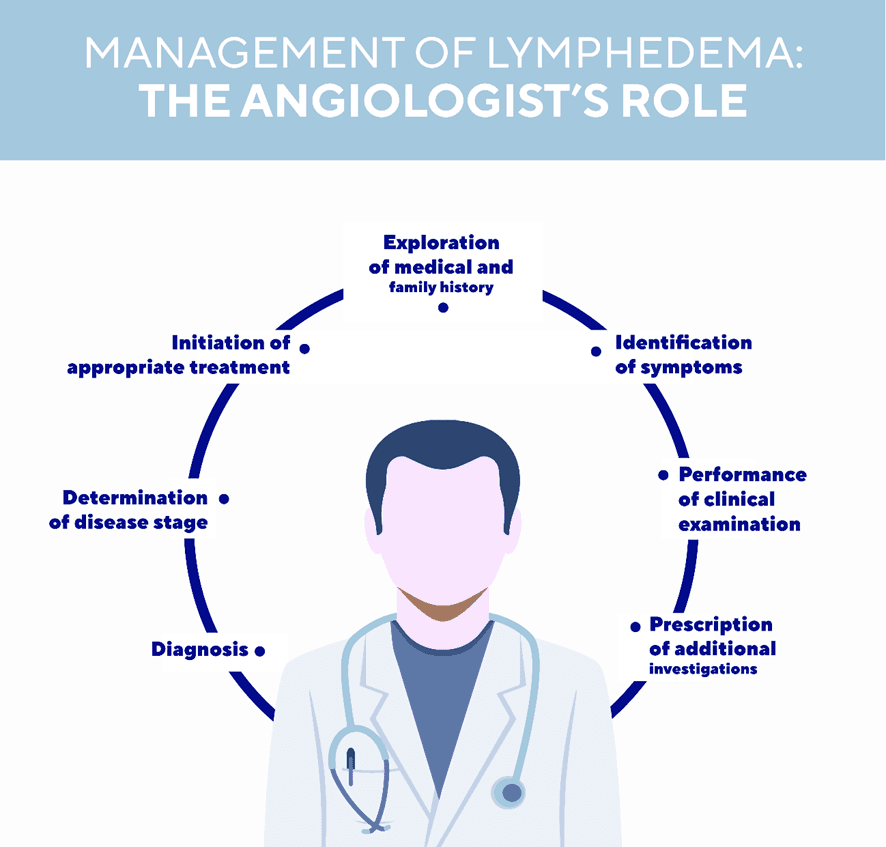
Angiolosts are doctors specialising in diseases of the blood and lymphatic vessels. They play a central role in the diagnosis and management of lymphedema.
A consultation will be conducted in several stages to help determine the possible causes of the condition, the type of lymphedema to be treated and its stage. What is the procedure during a consultation?
The interview phase
Diagnosing lymphedema is not always easy and requires the expertise of a specialist(1).
The first phase of the medical consultation is based on a series of questions. Different possibilities need to be eliminated by the angiologist to make sure the problem really is lymphedema. The interview allows the doctor to explore the patient’s personal medical history (history of cancer, for example, or erysipelas, in particular) and family history, along with his or her symptoms. This information will help guide the medical diagnosis towards primary or secondary lymphedema.
Primary lymphedema, which is rarer, is related to abnormal development of the lymphatic system from birth. In the majority of cases, it develops before the age of 35 but it may sometimes be detected later(2). Secondary lymphedema, which is much more common, is due to obstruction or destruction of the lymphatic vessels following cancer; an infection, surgery, radiotherapy, chronic venous insufficiency or even obesity(3).
The auscultation phase
A clinical examination will enable the angiologist to make an initial diagnosis. He or she may order additional investigations to confirm the diagnosis, such as lymphoscintigraphy, MRI or Doppler ultrasound(4). These investigations are always performed in addition to the clinical examination and are not enough in themselves to make an isolated diagnosis(5).
The doctor must also examine the condition of the skin, look for signs such as pitting, map the area affected, look for any comorbidities, such as venous disease or a venous ulcer, and eliminate any vascular contraindications to compression therapy. It is essential to measure the systolic index at the foot before initiating any compression of the lower limb.
Measurement of arm diameters by the angiologist will also enable estimation of the limb volume and the percentage difference compared to the volume of the opposite arm.
This percentage helps grade the severity of any limb edema and to determine eligibility for complex decongestive therapy. There are 4 clinical stages in lymphedema, going from 0 to 3(6) depending on whether or not the edema can be reduced and the condition of the skin:
- Stage 0: latent symptoms
- Stage 1: spontaneous reduction of edema at rest or when the affected limb is elevated
- Stage 2: presence of edema that does not spontaneously reduce, development of skin lesions
- Stage 3: very marked increase in limb volume, known as elephantiasis(6)
The treatments that may be prescribed by the angiologist
The angiologist may prescribe combined decongestive therapy to reduce the volume of the edema and prevent complications(7). These specialists always monitor the patient to make sure treatment is being correctly implemented and readjust it if required. Their role is to make a diagnosis and refer the patient to reference centres or physiotherapists qualified to treat lymphedema. They make sure that the right compression therapy is prescribed, that these devices are correctly used and that the patient is exercising and following lifestyle and dietary advice. They play a crucial role in the prevention of complications.
Antibiotics may be prescribed in the event of infectious complications (such as erysipelas) or as preventive treatment. In rare cases, an angiologist may recommend surgical treatment(8).
If you have any questions, ask your doctor for advice.
- Lymphedema causes, diagnosis and complications. angiologist.com website.
- Le lymphœdème primaire [Primary lymphedema] – November 2007 – Document produced with the collaboration of Doctor Stéphane Vignes / consultation of the rare vascular diseases reference centre / Cognacq-Jay Hospital, Paris
- Les lymphœdèmes des membres : diagnostic, exploration, complications [Lymphedema of the lower limbs: diagnosis, exploration, complications] – S. Vignes, M. Coupé, F. Beaulieu, L. Vaillant, for the “Recommendations” group of the Société Française de Lymphologie [French Lymphology Society] – Journal des Maladies Vasculaires (2009) 34, 314-322
- Bongard O. Lymphœdème des membres inférieurs. Le point de vue de l’angiologue [Lymphedema of the lower limbs. The angiologist’s perspective]. Revue Médicale Suisse, 2002. Volume 2, 22155
- Lee BB et al. Diagnosis and treatment of primary lymphedema. Consensus document of the International Union of Phlebology (IUP)-2013. Int Angiol. 2013 Dec;32(6):541-74.
- Rapport d'évaluation technologique : Lymphœdème et raideur de l’épaule après traitement d’un cancer du sein - Rapport d’évaluation [Technological Assessment Report - Lymphedema and shoulder stiffness following breast cancer – Assessment report] – HAS [French National Authority for Health], December 2012
- Lymphœdème primaire [Primary lymphedema]. Protocole National de Diagnostic et de Soins (PNDS -French national diagnosis and care protocol).Centre national de référence des maladies vasculaires rares [National reference centre for rare vascular diseases]. February 2019
- Chardon-Bras M and Coupé, M.Prise en charge et physiothérapie du lymphœdème des membres [Physiotherapy management of lymphedema of the limbs]. Revues générales. Cancérologie. “réalités cardiologiques” [cardiological realities] website


