Osteoarthritis of the thumb: understanding rhizarthrosis
Osteoarthritis of the thumb: symptoms
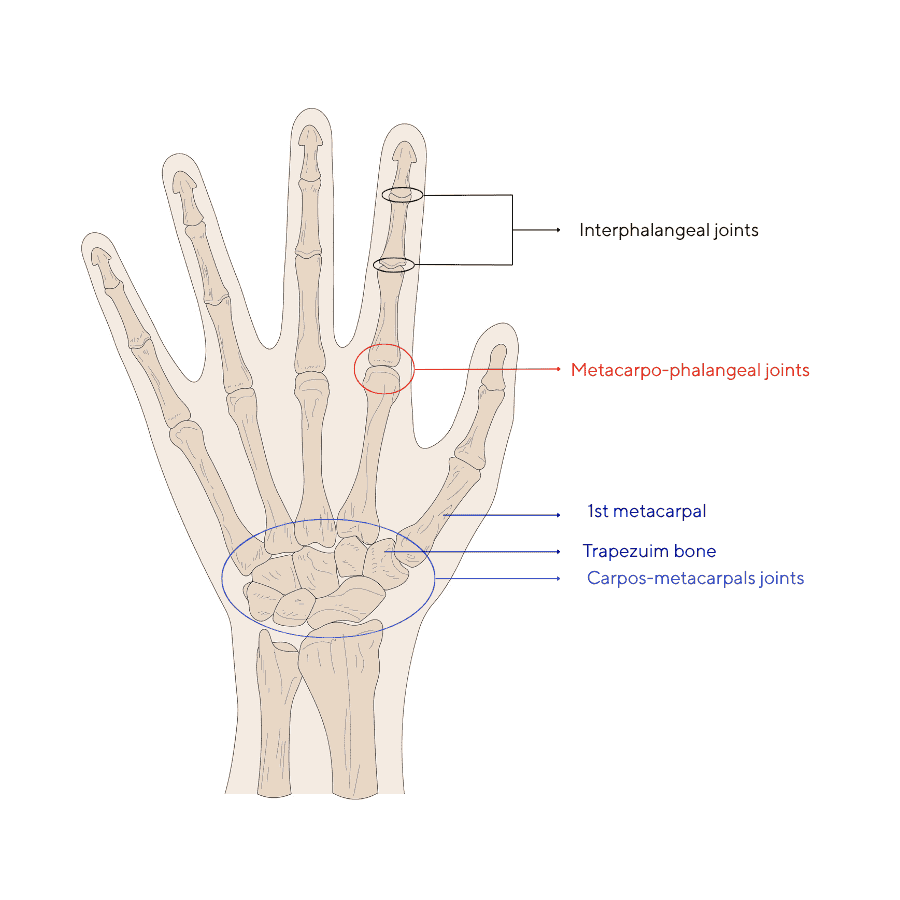
The thumb alone accounts for nearly 40% of the hand's function(1). Thanks mobility, it allows us to grasp and pinch, and makes most everyday movements possible. But this versatility comes at a price: the joint at the base of the thumb, called the trapeziometacarpal (or carpometacarpal) joint, is one of the most heavily used joints in the body. This is where thumb osteoarthritis, also known as rhizarthrosis, occurs.
What is rhizarthrosis?
Rhizarthrosis is the progressive wear and tear of the cartilage that covers the bone surfaces between the trapezium (a bone in the wrist) and the first metacarpal (base of the thumb).
When this cartilage deteriorates, the bones rub against each other, causing inflammation, pain and stiffness. As the disease progresses, deformities may appear, such as a "Z" thumb, which is typical of advanced forms. This deformity is linked to a subluxation of the metacarpal bone, an adduction (forward movement towards the inside of the hand) of the thumb towards the palm and a closure of the commissure between the thumb and index finger(1).
Osteoarthritis of the thumb: symptoms
The first signs of rhizarthrosis often go unnoticed: discomfort when opening a jar, turning a key or carrying heavy objects. Then the pain becomes more frequent, sometimes continuous, and can interfere with sleep.
The main symptoms include:
- pain at the base of the thumb, sometimes radiating to the wrist;
- a loss of grip strength, making it difficult to squeeze or pinch;
- joint stiffness, especially in the morning;
- visible deformation of the thumb in advanced cases;
- sometimes muscle atrophy at the base of the thumb.
Causes and risk factors(1,2)
Rhizarthrosis is most often the result of ligament laxity in the trapeziometacarpal joint2 . This hyperlaxity leads to increased mechanical stress on the joint, causing progressive cartilage loss, bone impingement and pain.
Other factors to an increased risk of developing this condition, such as:
- gender, women being more affected, probably due to hormonal factors such as the menopause(1,2);
- age, with the disease generally appearing after the age of 70(1) ;
- repetitive movements involving the thumb; thumb osteoarthritis is a known occupational disease (sewing, gardening, music, manual labour) 3;
- a history of thumb trauma(1) ;
- a family history of osteoarthritis.
Progression of the disease: the Eaton-Littler classification(5)
Although generally diagnosed by a general practitioner , the severity of rhizarthrosis is often assessed radiologically using the Eaton-Littler classification, stage IV of which has been modified by Eaton and Glickel . It describes four stages of progression:
Stage I – Early wear: The first signs appear: the joint at the base of the thumb is slightly wider than normal, but without any visible wear.
Stage II – Moderate wear: The joint begins to wear slightly: the space between the bones narrows a little, the bone becomes denser and small cysts or small bony growths (osteophytes) less than 2 mm in size may appear.
Stage III – Advanced osteoarthritis: Wear becomes significant: the space between the bones is greatly reduced, the bones are thickened, with larger cysts and osteophytes (greater than 2 mm).
Stage IV – Extensive osteoarthritis: The osteoarthritis spreads: the same signs as in stage III are present, but another neighbouring joint (between the scaphoid and trapezium) is also affected.
This scale allows treatment to be tailored, from wearing a brace to surgery.
How can osteoarthritis of the thumb be relieved?
Medical treatment
In most cases, treatment begins with conservative measures.
Wearing a resting or functional orthosis helps to stabilise the joint and reduce pain while maintaining the mobility necessary for daily activities(1).
Analgesic or anti-inflammatory drugs may be prescribed during flare-ups(1,4). In cases of persistent inflammation, an intra-articular injection may provide temporary relief(1).
Finally, therapeutic exercises(1,4) prescribed by a physiotherapist or occupational therapist help to strengthen the hand, maintain flexibility and adopt the correct movements to limit stress on the thumb.
Surgical treatment(1)
When pain becomes unmanageable despite conservative treatment, surgery may be considered.
Trapeziectomy (removal of the trapezium bone) remains the most common procedure. It may be combined with tendon interposition to stabilise the thumb.
Other options exist, such as the insertion of a trapeziometacarpal prosthesis or, more rarely, arthrodesis (fusion of the bones). These procedures aim to eliminate pain and restore satisfactory function, with slightly reduced but stable mobility.
The essential role of orthotics
Orthoses are a mainstay of non-surgical treatment for rhizarthrosis.
Rigid splints are recommended at night or during inflammatory flare-ups to immobilise the joint.
Flexible, more discreet functional orthoses can be worn during the day to support the thumb while maintaining mobility.
They must be individually fitted by a healthcare professional to ensure comfort, effectiveness and proper joint alignment.
Living with rhizarthrosis
Although thumb osteoarthritis is a chronic condition, it is possible to maintain your quality of life with appropriate treatment.
Adopting protective measures — avoiding twisting, using ergonomic objects, maintaining hand flexibility — helps to limit pain and slow down progression. Applying heat locally can help relieve pain during flare-ups(4).
A coordinated approach between the doctor, physiotherapist and orthotist allows most patients to maintain a satisfactory level of independence in their daily lives.
- Colonna S, Borghi C Rhizarthrosis Part I: A Literature Review. Cureus. (January 25, 2024) 16(1): e52932. DOI 10.7759/cureus.52932 https://pmc.ncbi.nlm.nih.gov/articles/PMC10893956/pdf/cureus-0016-00000052932.pdf
- Gillis J., Calder K., Williams J., Review of thumb carpometacarpal arthritis classification, treatment and outcomes, . can J Plast surg 2011;19(4):134-138.
- M J W van der Oest et al., The prevalence of radiographic thumb base osteoarthritis: a meta-analysis, Osteoarthritis and Cartilage, 2021, Vol. 29, Issue 6, p. 785-792
- ACOEM hand, wrist and forearm disorders guideline 2023 [OnLine] consulted Sept 2025 https://www.dir.ca.gov/dwc/DWCPropRegs/2023/MTUS-Evidence-Based-Update-July/Hand-Wrist-Forearm-Disorders.pdf
- Kennedy CD, Manske MC, Huang JI. Classifications in Brief: The Eaton-Littler Classification of Thumb Carpometacarpal Joint Arthrosis. Clin Orthop Relat Res. 2016 Dec;474(12):2729-2733. doi: 10.1007/s11999-016-4864-6. Epub 2016 May 4. PMID: 27146653; PMCID: PMC5085928.
- Wajon A, Vinycomb T, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database of Systematic Reviews 2015, Issue 2. Art. No.: CD004631. DOI: 10.1002/14651858.CD004631.pub4. Accessed 06 November 2025


