Venous insufficiency: definition, factors and treatment

What is venous insufficiency?
Chronic venous insufficiency (CVI) is a progressive disease that affects the venous system of the lower limbs and is characterised by venous hypertension, poor venous return and a series of symptoms, including pain, swelling, skin changes and ulcerations in the most advanced stages of venous insufficiency.

How compression works
© Agence Nouveau MondeWhat are the risk factors for venous insufficiency?
Risk factors for venous insufficiency include age, gender, pregnancy (which can compress the veins and worsen symptoms), family history, obesity or being overweight (which increase pressure in the legs and slow venous return), lack of physical activity, smoking and a history of phlebitis.
Heat also dilates the veins and exacerbates the sensation of heavy legs, as does prolonged sitting or standing, which hampers venous return.
It's important to treat these circulation problems early to avoid suffering from them as we get older. The first person to contact is your GP, who can then refer you to an angiologist or phlebologist if necessary. To help you know when to seek medical advice, please see our article.

Risk factors of venous insufficiency
© Nouveau MondeWhat are the clinical signs of venous insufficiency?
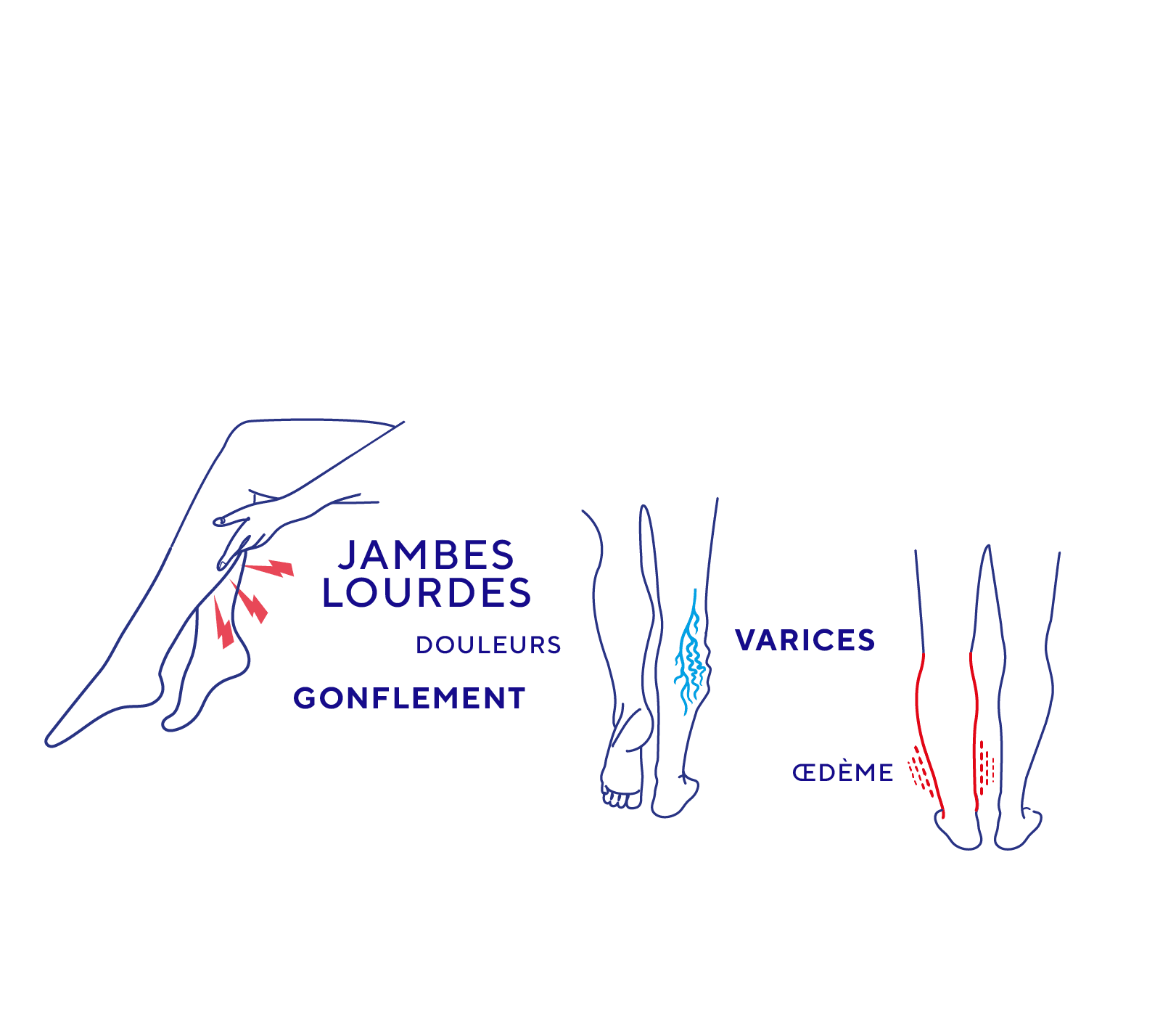
Common symptoms of venous insufficiency include a sensation of heavy legs, pain and swelling of the lower limbs, which generally intensifies at the end of the day or in hot weather (this swelling is known as oedema), and can progress to telangiectasia, reticular veins, varicose veins, oedema and skin changes (for example: hyperpigmentation, eczema, lipodermatosclerosis) and venous ulcers in the most severe cases of the condition(1, 2, 7 8).
It is essential to take these signs seriously and treat them carefully to prevent the condition from progressing too quickly.
What are the stages of chronic venous disease?
According to the Etiological Anatomical Physiopathological Classification (CEAP), chronic venous disease is classified into 6 stages in increasing order of severity.
The stages are defined as follows(3) :
- C0: No visible or palpable signs of venous disease.
- C1: Presence of telangiectasias or reticular veins.
- C2: Appearance of varicose veins.
- C3 : Development of oedema.
- C4 : Skin changes due to venous disease, with C4a indicating pigmentation or eczema, and C4b referring to lipodermatosclerosis or white atrophy.
- C5: Skin changes with a healed ulcer.
- C6: Skin changes with an active ulcer.
Did you know about venous insufficiency?
Chronic venous disease is widespread, affecting a significant proportion of the adult population, and its prevalence (number of cases in a population) increases with age(2,3).
Worldwide, this figure varies widely between continents, due to differences in lifestyle, and between the sexes. CVI is thought to occur in 1% to 40% of women and 1% to 17% of men.
Varicose veins are a much more common form of venous disease, occurring in between 1% and 73% of women and between 2% and 56% of men(21, 22).
What is the cause of venous insufficiency?
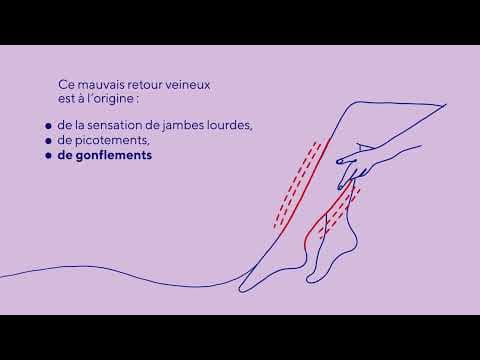
CVI is the consequence of venous hypertension due to a lack of tone in the veins and insufficient venous valves, which normally ensure that blood does not flow back into the veins(2,7).
This insufficiency of the venous valves leads to venous reflux and a reduction in the return of blood from the veins to the heart(2,7).
This poor venous return is at the root of the sensation of heavy legs, often accompanied by tingling, swelling and the other complications mentioned above (varicose veins, skin changes, ulcerations, etc.). Hypoxia and inflammation are also at the root of these complications(2,7).
The lack of tone in the veins and stagnation of blood in the legs leads to enlargement of the veins, forming varicosities which can vary in size and colour, from blue to black, and are accompanied by pain of varying intensity(2,7).
Venous insufficiency: the causes
© Nouveau mondeWhat are the possible complications of venous insufficiency?
Chronic venous insufficiency can lead to various complications.
First of all, venous insufficiency can become chronic, with complications that can be progressive: oedema, skin changes and the appearance of venous ulcers in the most advanced cases, which are difficult to treat(1,7,10).
Chronic venous insufficiency can also lead to serious complications, such as thrombo-embolic events. Venous thrombosis, also known as phlebitis, can develop(10) as a result of poor venous return and the accumulation of blood in the lower limbs, blood clots can form in a superficial or deep vein
Venous thrombosis can even be complicated by pulmonary embolism (if a clot forms in a deep vein, breaks loose and travels from the lower limbs to the lungs), a medical emergency that causes twelve thousand deaths every year in France(9).
Another complication is post-thrombotic syndrome. Post-thrombotic syndrome (PTS) is a chronic complication that occurs after deep vein thrombosis (DVT)(11). It develops in 20-50% of patients and has signs and symptoms in common with chronic venous insufficiency: pain, a feeling of heaviness in the legs, swelling (oedema) and altered skin, sometimes with ulcerations(12,13).
How is venous insufficiency treated?
All patients with signs and/or symptoms of CVI should first be treated conservatively. The use of compression stockings is the mainstay of this conservative management. However, risk modification such as weight reduction in obese patients, regular exercise such as walking, and smoking cessation should also be encouraged in patients.
Other treatment methods exist to manage CVI. There are drug treatments and, in some cases, surgical interventions(3).
If you have varicose or spider veins, or following surgery, your doctor may recommend the use of compression stockings. These are particularly beneficial for(15):
- Reduce pain and the feeling of heaviness in the legs,
- Reduce swelling in the lower limbs,
- Preventing the onset of venous thrombosis, especially during periods of prolonged inactivity following surgery or trauma,
- Avoid complications of thrombosis, such as post-thrombotic syndrome (pain and swelling in the leg).
In the early stages (C0 and C1), there is no evidence that venous compression can slow the progression of the disease. However, from stage C2 onwards, characterised by the appearance of varicose veins of 3 mm or more, venous compression becomes the treatment of choice. The strongest clinical evidence is for the treatment of open venous ulcers at stage C6(16,17).
Compression therapy is therefore an essential solution for combating venous insufficiency(17).
- Ruggiero, M., Grande, R., Naso, A., Butrico, L., Rubino, P., Placida, G., Cannistra', M., & Serra, R. (2016). Symptoms in patients with skin changes due to chronic venous insufficiency often lead to emergency care service: an Italian observational study. International Wound Journal, 13. https://doi.org/10.1111/iwj.12498.
- Eberhardt, R., & Raffetto, J. (2019). Chronic venous insufficiency.. Circulation, 130 4, 333-46 . https://doi.org/10.1161/CIRCULATIONAHA.113.006898.
- Youn, Y., & Lee, J. (2018). Chronic venous insufficiency and varicose veins of the lower extremities. The Korean Journal of Internal Medicine, 34, 269 - 283. https://doi.org/10.3904/kjim.2018.230.
- Gracia S, Miserey G, Risse J, Abbadie F, Auvert JF, Chauzat B, Combes P, Creton D, Creton O, Da Mata L, Diard A, Giordana P, Josnin M, Keïta-Perse O, Lasheras A, Ouvry P, Pichot O, Skopinski S, Mahé G. Update of the SFMV (French society of vascular medicine) guidelines on the conditions and safety measures necessary for thermal ablation of the saphenous veins and proposals for unresolved issues. J Med Vasc. 2020 May;45(3):130-146. doi: 10.1016/j.jdmv.2020.03.005. Epub 2020 Apr 15. PMID: 32402427.
- Chahim, M., Khider, L., Galloula, A., Mirault, T., & Messas, E. (2020, 3 mars). Insuffisance veineuse superficielle des membres inférieurs. EM Consulte. Doi : 10.1016/S2211-0364(19)78955-9 Consulté le 4 avril 2024, à l’adresse https://www.em-consulte.com/article/1353714/insuffisance-veineuse-superficielle-des-membres-in
- Lebreton-Legarçon, C., & KoÇak, F. (2020). L’insuffisance veineuse, une maladie chronique et évolutive. Actualités Pharmaceutiques, 59(594), 8‑12. https://doi.org/10.1016/j.actpha.2019.12.023
- Krizanova, O., Penesova, A., Hokynková, A., Pokorná, A., Samadian, A., & Babula, P. (2023). Chronic venous insufficiency and venous leg ulcers: Aetiology, on the pathophysiology-based treatment.. International wound journal. https://doi.org/10.1111/iwj.14405.
- Azar, J., Rao, A., & Oropallo, A. (2022). Chronic venous insufficiency: a comprehensive review of management.. Journal of wound care, 31 6, 510-519 . https://doi.org/10.12968/jowc.2022.31.6.510.
- Blanchemaison, P. (2017, 9 mars). La lettre de d’institut Européen de Physio nutrition : Prévenir et traiter l’insuffisance veineuse : intérêt de l’association d’une substance phlébotonique avec des antioxydants. Institut Européen de Physionutrition et de Phytothérapie. Consulté le 4 avril 2024, à l’adresse https://iepp-eu.com/wp-content/uploads/2013/04/Lettre-IEPP-n06-Insuffisance_veineuse.pdf
- Santler, B., & Goerge, T. (2017). Chronic venous insufficiency – a review of pathophysiology, diagnosis, and treatment. JDDG Journal Der Deutschen Dermatologischen Gesellschaft, 15(5), 538‑556.https://doi.org/10.1111/ddg.13242
- Haute Autorité de santé (HAS). La compression médicale dans le traitement de la maladie thrombo-embolique veineuse. Site internet : HAS, 2010
- Rabinovich, A., & Kahn, S. (2017). The postthrombotic syndrome: current evidence and future challenges. Journal of Thrombosis and Haemostasis, 15, 230 - 41. https://doi.org/10.1111/jth.13569.
- Kahn, S., Galanaud, J., Vedantham, S., & Ginsberg, J. (2016). Guidance for the prevention and treatment of the post-thrombotic syndrome. Journal of Thrombosis and Thrombolysis, 41, 144 - 153. https://doi.org/10.1007/s11239-015-1312-5.
- Araujo, D., Ribeiro, C., Maciel, Á., Bruno, S., Fregonezi, G., & Dias, F. (2023). Physical exercise for the treatment of non-ulcerated chronic venous insufficiency.. The Cochrane database of systematic reviews, 6, CD010637 . https://doi.org/10.1002/14651858.CD010637.pub3.
- Compression stockings : MedlinePlus Medical Encyclopedia. (2022, 21 juillet). National Library Of Medecine. Consulté le 4 avril 2024, à l’adresse https://medlineplus.gov/ency/patientinstructions/000597.htm
- Autorité de santé (HAS). La compression médicale dans les affections veineuses chroniques. Site internet : HAS. Saint-Denis La Plaine (France) ; 2010
- Debure, C. (2015). La compression veineuse dans l’insuffisance veineuse. Annales de Dermatologie et de Vénéréologie (Print), 142(8‑9), 469‑475. https://doi.org/10.1016/j.annder.2015.06.014
- Mościcka, P., Szewczyk, M. T., & Cwajda‐Białasik, J. (2016). The education of chronic venous insufficiency and ulceration patients on the compression therapy. Pielęgniarstwo Chirurgiczne I Angiologiczne/Surgical And Vascular Nursing, 2016(3), 79‑84. https://www.termedia.pl/Journal/-50/pdf-28557-10?filename=Edukacja.pdf
- Berszakiewicz, A., Sieroń, A., Krasiński, Z., Cholewka, A., & Stanek, A. (2020). Compression therapy in venous diseases : physical assumptions and clinical effects. Postępy Dermatologii I Alergologii, 37(6), 842‑847. https://doi.org/10.5114/ada.2019.86990
- Comment soigner l’insuffisance veineuse ? - VIDAL. (s. d.). VIDAL. https://www.vidal.fr/maladies/coeur-circulation-veines/jambes-lourdes/traitements.html
- Beebe-Dimmer, J. L., Pfeifer, J. R., Engle, J. S., & Schottenfeld, D. (2004). The Epidemiology of Chronic Venous Insufficiency and Varicose Veins. Annals Of Epidemiology, 15(3), 175‑184. https://doi.org/10.1016/j.annepidem.2004.05.015
- Vuylsteke, M., Colman, R., Thomis, S., Guillaume, G., Van Quickenborne, D., & Staelens, I. (2018). An Epidemiological Survey of Venous Disease Among General Practitioner Attendees in Different Geographical Regions on the Globe: The Final Results of the Vein Consult Program. Angiology, 69, 779 - 785. https://doi.org/10.1177/0003319718759834.


