Total knee replacement
Today, this common procedure provides satisfactory and long-lasting results for patients with osteoarthritis of the knee (or gonarthrosis). However, it is a major surgical procedure: it is crucially important to be well prepared for the surgery and to carefully follow the recommendations afterwards.
What is the purpose of a total knee replacement?
In a “total” knee replacement, the entire joint affected by the osteoarthritis is replaced by an implantable device. “Partial” - or “unicompartmental” - replacements, in which only a part of the knee joint is replaced, are more rare(1).
The main objective of a total joint replacement is to alleviate pain and restore good mobility of the knee(1). The surgeon and patient decide on the procedure together, on the basis of physical examinations and X-rays: the knee must demonstrate signs of major wear in all its compartments. The patient’s age, lifestyle and preferences also come into play.
In patients with OA of the knee (or gonarthrosis), a knee replacement is generally only considered when treatments are no longer able to alleviate the pain and reduce the level of disability day-to-day.(1)
Total knee replacement: a technically advanced operation
A total knee replacement - or arthroplasty - is a relatively common procedure, increasingly performed all around the world. As a result of population growth and ageing, the number of procedures of this type is increasing significantly and is expected to more than double by 2050(2).
Significant technical progress has been made in recent years in terms of implant design and materials. Prosthetic joints now have a lifespan of between 12 and 20 years(1). New surgical methods, including computer-assisted arthroplasty, have also emerged.
Different types and models of implants for total knee replacement
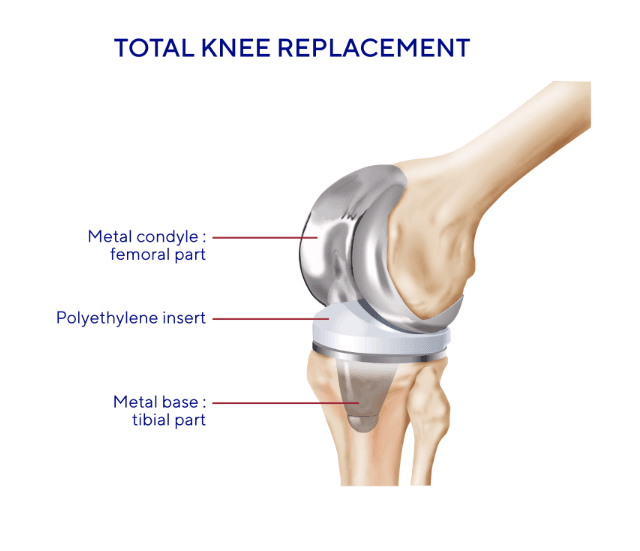
The most commonly used total knee joint replacements - or “tricompartmental” replacements - are “unconstrained” (or standard) prostheses. “Constrained” or “hinged” prostheses account for only a small proportion of joint replacements.
These implants are generally made of metal alloys, with polyethylene parts in the majority of unconstrained prostheses. They are manufactured by approved laboratories in accordance with very strict standards.
Surgeons select the implant type from the ranges proposed by manufacturers on the basis of patients’ anatomy and the condition of their ligaments and bones.
Joint replacement: from preparation to recovery
If possible, arthroplasty should be performed at a centre specialised in joint replacement surgery. Between the time when surgical treatment is decided upon and the time it is actually performed (generally several weeks), patients are usually asked to exercise in order to facilitate the recovery of mobility, smokers are asked to stop smoking to improve healing and overweight patients are asked to lose weight to relieve strain on the prosthetic joint. It is also important to clear up any sources of infection, however modest (dental problems, sinusitis, etc.), to prevent any germs getting into the prosthetic joint.
Preparation
Knee joint replacement is a common procedure but it is still major surgery that needs to be carefully prepared, with, in particular:
- A pre-operative assessment
- Anticoagulant treatment
- Antibiotic treatment to combat any risk of infection.
The surgery(3):
- Duration: Performed at the hospital, and last 1 to 2 hours.
- Anesthesia: A general anaesthetic is performed. A spinal or locoregional anaesthetic (when only the lower half of the body or the leg are put to sleep) is also possible.
- Incision and Removal: The surgeon makes an incision on the front of the knee, then removes the damaged cartilage and osteophytes (bony outgrowths).
- Bone Preparation: The surgeon shapes the tibia and femur to accommodate the prosthetic components.
After the surgery:
- Medication: Painkillers, anti-inflammatories and anticoagulant are prescribed.
- Hospital stay: Most patients have a brief recovery period in the hospital, with many able to return home on the same day as the surgery(3).
- Physical therapy: It is important to move the new joint after the surgery, so a physical therapist will plan an exercise plan for you(3).
- Mobility aids: To prevent falls, you may be provided with a cane or walker(3).
- Wound care: Keep the surgical area around your knee clean and dry(3).
Back home
It is essential to follow the doctor’s instructions, concerning, for example, wound hygiene or nursing care, the treatments to be taken (anticoagulants, wearing of compression stockings for around 4 to 6 weeks), physiotherapy, follow-up examinations and consultations, etc.
It is recommended that patients go up and down stairs one step at a time for the first few weeks and that they take care when carrying out their routine activities (bath, moving around, getting dressed). Allow yourself a convalescence and adjustment period of 2 to 3 months. Tell your doctor straight away if you have any swelling, if your wound weeps or if you experience pain, fever or abnormal redness.
You may return to work after between 1.5 months (in the event of a sedentary job) and 4 months (in the event of a physically strenuous job). Depending on your line of work, it may be necessary to adapt your job or retrain. It is possible to begin sports activities again gradually from the 3rd month (walking, swimming, cycling, etc.), avoiding sports that cause significant impacts on the knee.
If you have any questions, ask your doctor for advice.
- Informations pratiques - La prothèse de Genou - Société Française de Chirurgie Orthopédique et TraumatologiqueUnaformec - Gonarthrose https://www.sofcot.fr/sites/www.sofcot.fr/files/medias/documents/18-442.pdf
- Hannouche, D., Diogo, V. C., Miozzari, H., & Lübbeke, A. (2017b, décembre 13). La prothèse totale du genou répond-elle aux attentes des patients ? Revue Medicale Suisse. https://www.revmed.ch/revue-medicale-suisse/2017/revue-medicale-suisse-587/la-prothese-totale-du-genou-repond-elle-aux-attentes-des-patients
- Total knee replacement - OrthoInfo - AAOS. (s. d.). https://orthoinfo.aaos.org/en/treatment/total-knee-replacement
Crédit d’illustration : Thuasne


